What is a Pachymeter?
Precision matters in eye care, especially when corneal thickness can influence pressure readings and surgical decisions. Pachymetry measures corneal thickness in micrometers (µm). It helps interpret applanation IOP readings, informs glaucoma risk, supports refractive surgery planning, and assists in evaluating corneal disease over time.
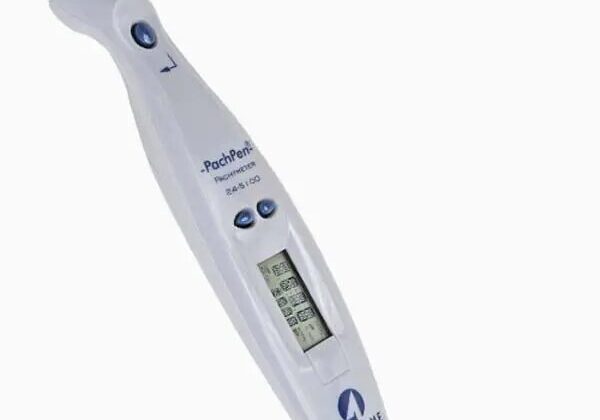
If you’ve ever wondered what exactly a pachymeter is, it’s the device that makes these measurements possible with reliable, clinic-ready accuracy. In the sections ahead, we’ll compare ultrasound and optical approaches, when to use each in the clinic, and how pachymetry adds clinical context alongside tonometry and corneal imaging.
Quick Answer: What Does a Pachymeter Do?
A pachymeter measures corneal thickness in micrometers (µm). It adds critical context to applanation IOP readings, helps evaluate refractive surgery candidacy, and supports ongoing monitoring of corneal disease. It’s quick and repeatable in routine clinic use, and is available as non-contact optical (e.g., AS-OCT or rotating Scheimpflug) or brief-contact ultrasound, so you can match the method to your workflow and patient comfort, supporting baseline measurements and follow-up comparisons over time.
What Is Pachymetry?
Pachymetry measures corneal thickness in micrometers (µm). In clinics, this is captured with handheld ultrasound pachymeters or non-contact optical systems such as anterior-segment OCT and rotating Scheimpflug tomography.
Key differences:
- Corneal topography maps corneal shape/curvature; pachymetry measures thickness. Some platforms (e.g., Scheimpflug tomographers) report both in one scan.
Knowing precise corneal thickness helps your provider interpret applanation IOP correctly and evaluate LASIK candidacy, since insufficient residual stromal thickness increases ectasia risk.
Why Measure Corneal Thickness?
Measuring corneal thickness plays a key role in eye health:
- Accurate IOP interpretation
- With Goldmann applanation tonometry, thicker corneas typically overestimate IOP and thinner corneas underestimate it. Pachymetry provides the context clinicians need when assessing glaucoma risk.
- Pre-surgical evaluation
- Confirms adequate residual stromal bed for LASIK/PRK.
How Does Pachymetry Work?
There are two main approaches: ultrasound pachymetry and optical pachymetry (e.g., anterior-segment OCT or rotating Scheimpflug tomography). Each method carries trade-offs in speed, comfort, infection-control workflow, and cost. Below is how each technology behaves in day-to-day clinic use.
Ultrasound Pachymetry
- Anesthetic drops numb your eye.
- A handheld probe makes brief contact with the cornea; multiple readings are typically averaged for a stable central value.
- Many handheld ultrasound pachymeters list accuracy around ±5 µm (device-dependent), which is appropriate for routine clinic use.
- Quick (typically well under a minute per eye) and cost-effective for point-of-care measurements.
- Requires cleaning and disinfection of the probe tip between patients per manufacturer and clinic protocol.
Optical Pachymetry (OCT/Scheimpflug)
- Non-contact optical imaging maps corneal thickness using AS-OCT interferometry or rotating Scheimpflug tomography (e.g., Pentacam-type systems).
- No anesthesia needed; more comfortable for you.
- Provides non-contact thickness maps across the cornea.
Choose the approach that fits your workflow and patient comfort; Insight Eye carries both handheld ultrasound pachymeters (e.g., Accutome PachPen, AccuPach VI) and multi-modal ultrasound platforms (e.g., Accutome 4Sight).
Preparation and What to Expect
Before your pachymetry test, here’s what to expect and how to prepare:
- No special fasting or diet changes are needed.
- Remove contact lenses as directed: recent lens wear can cause short-term corneal thickness changes that may affect readings.
- Ultrasound pachymetry: your provider places numbing drops, then a handheld probe briefly touches the cornea, several quick readings are averaged; the process typically takes well under a minute per eye.
- Optical pachymetry (AS-OCT or rotating Scheimpflug): you rest your chin and forehead on the support; the system captures a quick, non-contact scan.
- Risks: ultrasound involves brief contact, so irritation is uncommon and infection risk is low when the probe is properly disinfected between patients; optical imaging is non-contact.
Final Thoughts on How Pachymetry Works and Why It Matters
Understanding and using pachymetry can sharpen glaucoma risk assessment, guide refractive surgery planning, and support corneal disease management. Talk with your provider about when pachymetry fits your exam and how the numbers will be used, whether that’s interpreting IOP, planning refractive surgery, or tracking corneal change over time.
Have questions or need a device recommendation? Reach out to us for guidance, pricing, and availability.
